Sept. 16, 2020
Tips on managing stress and anxiety during transitional times in the pandemic

The beginning of fall can signal the start of a new year for many of us, but this one feels markedly different. Whether it’s continuing the work- or study-from-home marathon, or preparing to re-enter workplaces, schools, or lecture halls, stress and anxiety, among other mental health concerns, can run high. Professor of clinical psychology and UCalgary Depression Research Laboratory lead Dr. Keith Dobson, PhD, recently shared knowledge from his practice, and talked about the challenges that affect us all in transitional times during the pandemic.
Be aware of precipitating risk factors
“Risk can take many different forms. There’s typically not one single factor that causes or explains mental health problems or mental illness for any one person.” Dobson reviewed biological, psychological, and social risk factors that can contribute to risk. Particular risks mentioned as it pertains to the COVID-19 context include: sleep dysregulation, reactions to stress, worry and rumination, escape or avoidant behaviour, relationship tension, and lack of social support, among others.
With this in mind, Dobson advocates for balancing or even reducing these risk factors through protective factors that build resilience, or if need be, seeking professional help.
Build resilience through protective factors
Dobson mentioned several protective factors that can help build resilience.
- Balanced and recuperative temperament
- Physical well-being/ regular sleep, eating and exercise
- Coping strategies; it is better to approach, rather than avoid problems
- Social and personal competence
- Positive peer relationships
- Positive family relationships
Among these six factors, Dobson highlighted several areas to consider, given our COVID-19 context.
Regulate and create routines as best as we can given our varying environments. Eat, sleep, work, and exercise as regularly as possible. When in study or work mode, create mini-breaks away from the screen (e.g., an invigorating walk or a small snack) to combat digital fatigue, and that will energize or better prepare you to come back to a task.
Watch your self-talk. “The way you talk to yourself matters,” Dobson explains. “If you’re saying things that are negative and pessimistic, you’ll probably tend to look for things that are negative in your environment. If you can challenge those thoughts with good evidence or replace them with positive thoughts that work for you, this can help quite a bit. If you notice you’re ruminating, pay attention to the content and process of rumination: when does it occur, are certain people triggering you, do you tend to ruminate after you watch the news? These might be clues in how you can change the process in how you’re engaging with your environment.”
Turn down the media noise. Find a reputable source or two and decide how much time you’re comfortable getting news updates. Dobson suggests that if you’re looking for reputable health information, instead of news media, look at public health bodies like Public Health Agency of Canada, Health Canada, Provincial Ministries of Health, and World Health Organization.
Schedule activities. Schedule at least one activity each day that gives you pleasure and another that gives a sense of purpose. Activities can be anything that works for you, such as accomplishing a task, or engaging in a hobby you enjoy. Dobson also suggested finding a hobby or cause “bigger than ourselves” as a way to find purpose.
Keep social contact. “Even though we have to physically distance, we shouldn’t be engaging in social distance,” Dobson advocates. “Stay in contact with the people you know and love.”
How do we know when we need to seek help?
Sometimes it’s hard or impossible to engage in the protective behaviours mentioned above. In this case, it might be necessary to find more formal support. So how do we know when to seek help?
To check in with ourselves, Dr Dobson suggests using the Mental Health Continuum Model — a framework that can be used to pinpoint our mental health, which can fluctuate along a spectrum (in this case from green to red, healthy to ill). The continuum includes different signs and indicators people express that indicate how they are functioning.
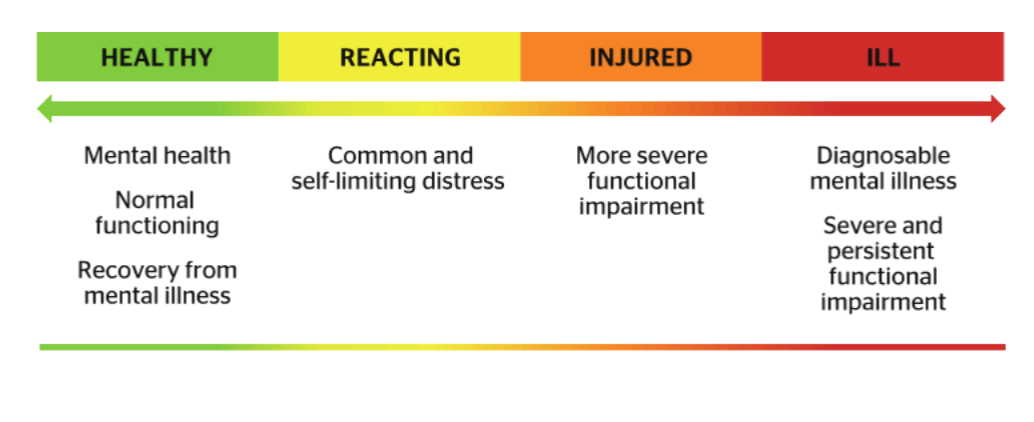
If you have noticed a shift in your signs and symptoms, or you are moving into the orange or red zones, formal treatment might be a solution that’s right for you. It might take a bit of time, but finding the right treatment is important and the earlier you can seek treatment the better the outcome.
At UCalgary, we are still here to support you, even if you’re not on campus. Mental health services and supports are available for students, faculty and staff. Find support here.
If you are a member of the UCalgary community and would like to learn more about the Mental Health Continuum, sign up for The Inquiring Mind (for students) or The Working Mind (for faculty and staff).
This article is a recap of a previous webinar. If you’d prefer to watch the webinar, view it below, or browse Dr. Dobson’s slides as well as resource links here.
The University of Calgary’s Campus Mental Health Strategy is a bold commitment to the importance of mental health and well-being of our university family. Our vision is to be a community where we care for each other, learn and talk about mental health and well-being, receive support as needed, and individually and collectively realize our full potential. Learn more about the strategy here.



